Pelvic pain is one of the most common complaints among women, yet it is often brushed aside as “just part of being a woman.” But what if that persistent pain is not just cramps, stress, or something you ate? Could it be a deeper condition - one that silently affects millions of women worldwide? That condition is endometriosis
Understanding Endometriosis
Endometriosis is a condition that often remains undiagnosed in the majority of cases. It is a chronic condition in which endometrial cells move out of the uterus, to other organs which can lead to estrogen-driven inflammation. The extent of the disease can vary ranging from peritoneal deposits to endometrial cells invading other organs such as the bladder, bowel, ureter etc.
This “migration” of endometrial tissue is what makes endometriosis so complex and difficult to treat. Instead of shedding away like normal menstrual lining, these misplaced cells bleed internally, cause inflammation, and eventually lead to scarring and adhesions. Over time, this cycle can cause debilitating pain and, in many cases, fertility issues.
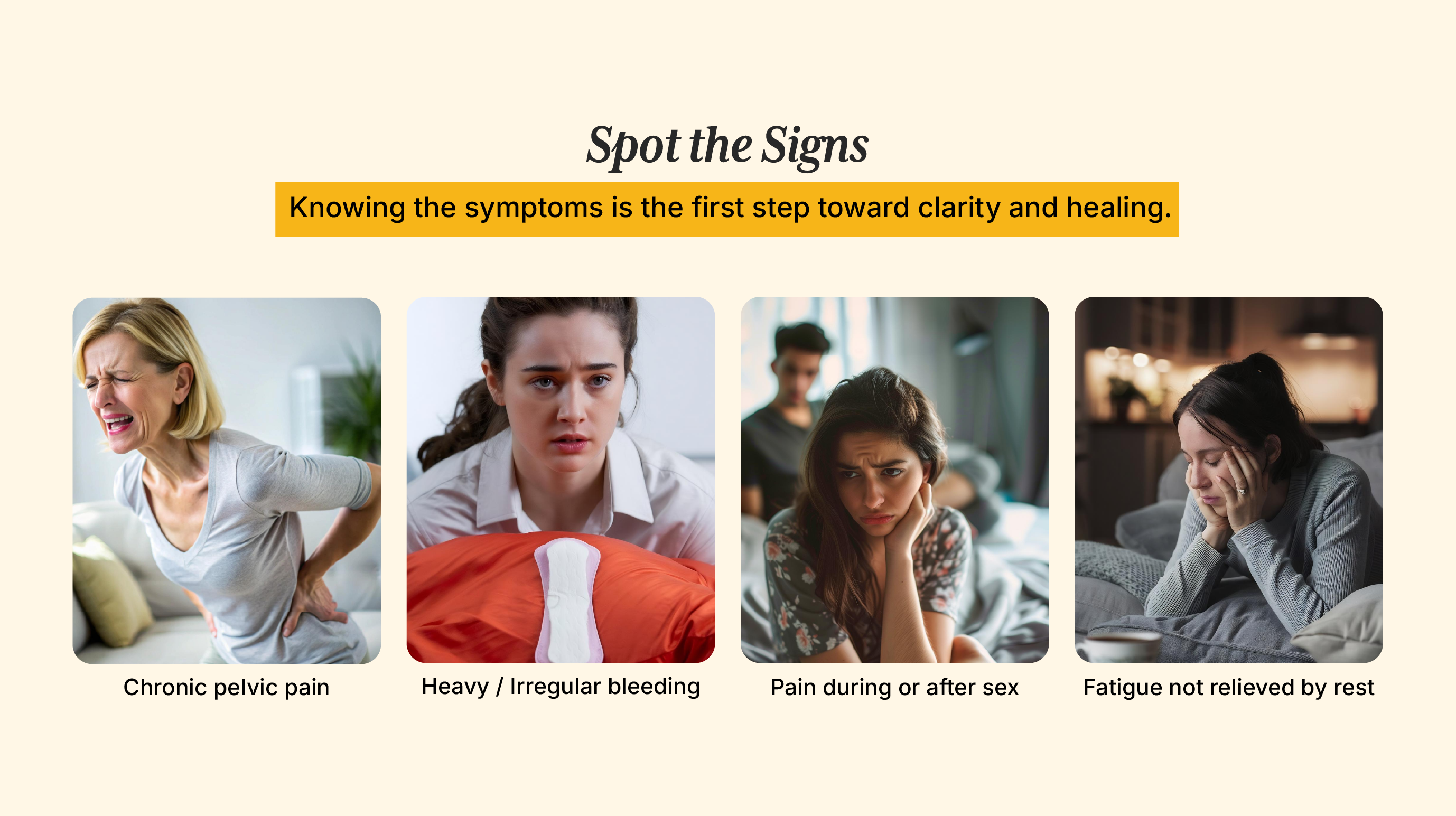
Recognizing the Symptoms
The symptoms include pelvic pain without menstruation, irregular periods, painful intercourse, bowel and bladder symptoms and fatigue. Symptom severity does not depend on the extent of the disease, as some individuals can be asymptomatic, which makes the diagnosis of the condition difficult.
Common Signs of Endometriosis
- Chronic pelvic pain that doesn’t go away after periods.
- Irregular cycles or abnormally heavy bleeding.
- Pain during or after intercourse.
- Digestive issues such as constipation, bloating, or diarrhea during menstruation.
- Fatigue that isn’t relieved by rest.
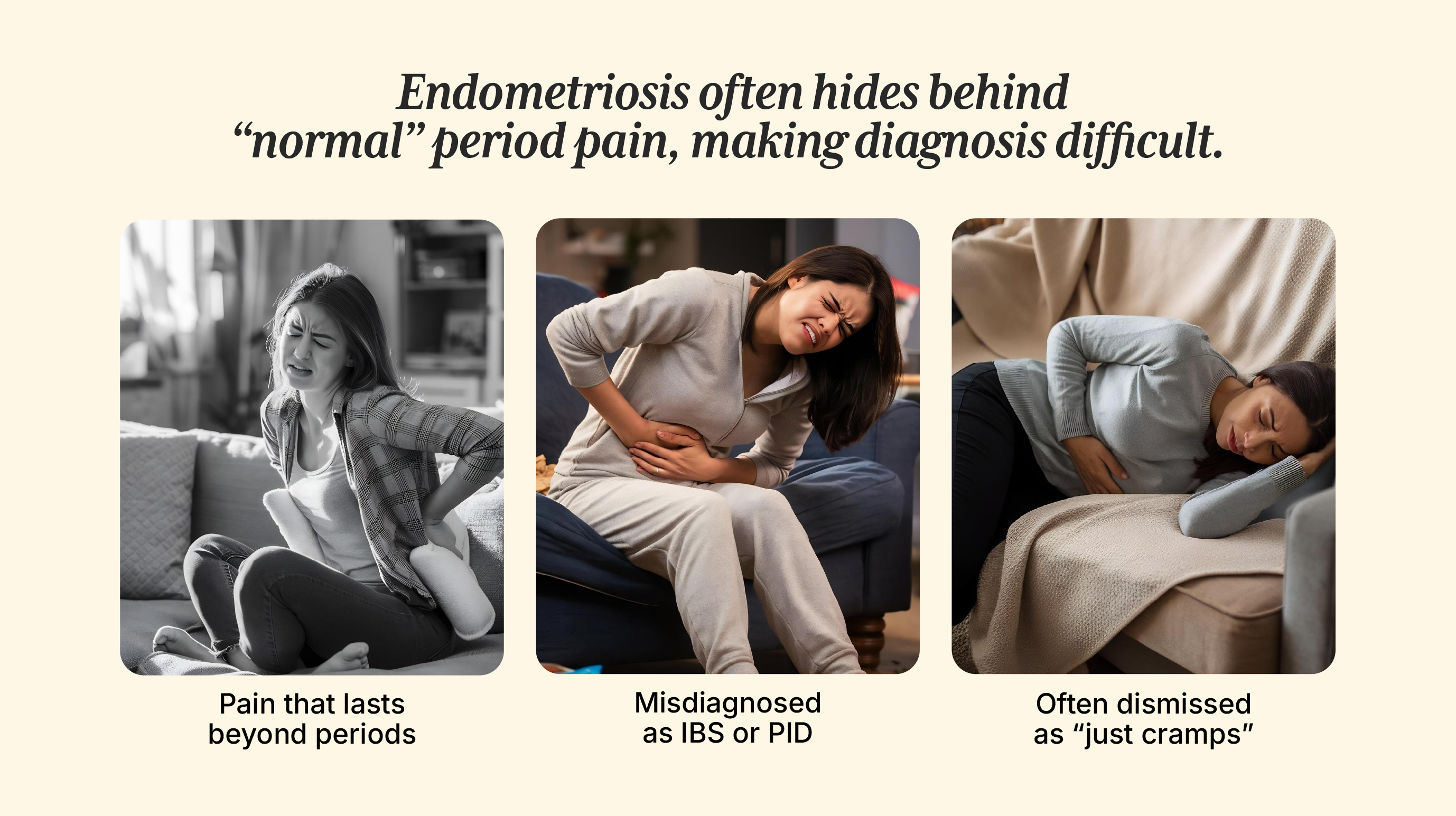
Because symptoms can overlap with other conditions like irritable bowel syndrome (IBS) or pelvic inflammatory disease (PID), women may spend years seeking answers before receiving a proper diagnosis.
What Causes Endometriosis?
The cause of the endometriosis is not definitive. The most common theory is of retrograde menstruation (the endothelial cells, rather than going down the uterus, go into the fallopian tubes, get implanted, and multiply there).
There are various factors for abnormal cellular proliferation, including genetic, hormonal, and immune dysregulation. The endometrial cells respond to estrogen stimulation, leading to inflammation, scarring, further adhesions, and cluster formation.
Possible Contributing Factors
- Genetics – Women with a family history are more likely to develop the condition.
- Hormonal imbalance – High estrogen levels can fuel the disease.
- Immune dysfunction – Some women’s immune systems may fail to clear misplaced cells effectively.
- Environmental triggers – Exposure to toxins and endocrine disruptors could play a role.
Risk Factors You Should Know
The risk factors include low birth weight, Mullerian anomalies, early menarche, short menstrual cycles, increased menstrual flow, low body mass index, and nulliparity.
While these factors do not guarantee the condition, being aware of them can help women take charge of their health earlier and advocate for proper medical attention.
Why Endometriosis Often Goes Undiagnosed
Endometriosis has a high rate of being undiagnosed, as the pelvic pain is regarded as ‘normal menstrual pain.’
The Silent Struggle
There are other symptoms that will help distinguish it from cramps. These symptoms include:
- Severity and persistence of pain: While typical period cramps are often mild to moderate and manageable with over-the-counter pain relievers, endometriosis pain is frequently described as severe, excruciating, or debilitating. This pain can last for more than the duration of periods.
- Pain beyond menstruation: The pain related to endometriosis can last six months or more. The pain can be felt during intercourse, painful bowel movements or urination, especially during periods, or lower back or abdominal pain that is not directly related to menstrual flow.
- Associated symptoms: Other symptoms include difficulty getting pregnant, fatigue, heavy or irregular periods, and GI symptoms such as diarrhea, bloating, constipation especially during periods.
The misconception that “painful periods are normal” is one of the reasons why endometriosis goes undetected.
The Role of Awareness
Women should keep track and observe their flow, menstrual and/or pre-menstrual symptoms, duration of periods and cycle. This habit will help them to identify changes in their cycle or observe presence of new or worsened symptoms.
There exists a lack of awareness among patients and sometimes even doctors. This is due to:
- Normalization of pain
- Difficulty differentiating symptoms
- Stigma related to menstruation
- Use of pain relief instead of finding the root cause of the pain
- Misdiagnosis
Breaking this cycle requires education, open conversations about menstrual health, and better diagnostic support in healthcare systems.
Treatment Options
Treatment options for endometriosis include:
- Pain medication – To temporarily relieve discomfort.
- Hormone therapy – To suppress estrogen and slow the growth of endometrial tissue.
- Fertility treatment – For those struggling with conception.
- Hysterectomy with removal of the ovaries – A last-resort option for severe cases.
Modern medicine focuses on symptom management, but functional approaches that address the root cause are becoming increasingly important.

The Role of Nutrition in Endometriosis Management
Nutritional management include:
- Eliminating inflammatory food such as processed foods, soy, gluten, sugar etc.
- Incorporating anti-inflammatory foods such as omega-3 rich fish, colorful fruits and vegetables that are rich in antioxidants, fiber-rich foods such as whole grains, legumes etc.
- Reducing exposure to Xenoestrogens (found in plastics, cosmetics etc.), as elevated estrogen levels can worsen symptoms and disease severity.
- Low FODMAP diet has also been shown to have beneficial effects.
Why Diet Matters
Food has the power to either fuel inflammation or fight it. For women with endometriosis, adopting an anti-inflammatory diet and lifestyle can significantly improve quality of life and reduce dependency on medications.
Living With Endometriosis
While there is no permanent cure yet, many women manage their symptoms and lead fulfilling lives by combining medical treatment with lifestyle changes such as:
- Regular exercise to reduce inflammation.
- Mind-body practices like yoga and meditation.
- Adequate sleep and stress management.
- Building a strong support network of family, friends, and healthcare providers.
Final Thoughts
Pelvic pain is not something to brush aside. If you experience severe or persistent discomfort, it’s worth asking: “Could this be endometriosis?” Early diagnosis and proactive management can change the trajectory of a woman’s health, fertility, and overall quality of life.
By spreading awareness and normalizing the conversation around women’s pain, we can help countless women break free from silent suffering.
At iThrive, we specialize in root-cause healing through functional nutrition and lifestyle interventions tailored to your unique body.
Book a free consult with iThrive today and take the first step toward clarity, relief, and thriving health.
REFERENCES
Pathophysiology, diagnosis and management of endometriosis - https://www.bmj.com/content/379/bmj-2022-070750.abstract
Diagnosis and management of endometriosis - https://www.cmaj.ca/content/195/10/E363.short
Pathogensis based diagnosis and treatment of Endometriosis - https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2021.745548/full
Dietary and Nutritional Interventions for the Management of Endometriosis - https://pmc.ncbi.nlm.nih.gov/articles/PMC11643425/#sec4-nutrients-16-03988
Low FODMAP diet can easy symptoms of those with Endometriosis study - https://www.monash.edu/news/articles/low-fodmap-diet-can-ease-symptoms-of-those-with-endometriosis-study
Subscribe to our newsletter and receive a selection of cool articles every week



.png)


.webp)

.jpg)
.jpg)