Research shows that Indians spend an average of 9-10 hours a day sitting and this sedentary lifestyle has quietly become one of the biggest causes of metabolic issues like insulin resistance, diabetes and weight gain. In fact, a global study published in Diabetologia found that people who sit for more than 8 hours a day have up to 90% higher risk of developing Type 2 Diabetes.
This isn’t just about being overweight or eating unhealthy food. Even if you look fit, sitting for long hours slows down your metabolism, reduces how well your body uses insulin, and can lead to stubborn belly fat or constant fatigue.
It’s not just your body that’s affected. Long hours of screen time, poor posture, and continuous stress overload can also impact your brain, leading to mood swings, brain fog and reduced focus.
In this blog, we’ll break down what insulin resistance really means, how your long sitting hours are affecting your overall health, from metabolism to mental well-being, and most importantly, what simple changes you can make to prevent it.
What Is Insulin Resistance?
Whenever you eat food, especially carbs like rice, roti or fruit, your body breaks it down into glucose (sugar). This glucose travels through your blood and gives you energy to work, think, and move. Now, there’s one important hormone that helps this process and that is insulin.
It’s made by your pancreas and acts like a key that unlocks your cells so glucose can enter and be used as fuel. But when you sit for long hours, eat at irregular times, or are under constant stress, your cells slowly stop responding to insulin’s “knock.” So even though your body keeps making insulin, your cells don’t let glucose in. This is called insulin resistance, where your cells ignore insulin’s signal and block glucose from entering.
As a result, glucose stays in your blood instead of being used for energy. Over time, your body starts producing more and more insulin to compensate leading to fat storage (especially around the belly), fatigue, sugar craving, and weight gain.
Check out our blog on: Signs of Insulin Resistance | Understanding the Silent Threat
How a Desk Job Contributes to Insulin Resistance

Long hours of sitting, constant deadlines, and screen overload can affect how your body uses energy, responds to insulin, and even how your brain functions. Here’s how it happens:
1. Slow Metabolism
When you sit for long hours, your largest muscles, especially in your legs and back, stay inactive. These muscles normally help your body use up glucose for energy. But when they’re not moving, glucose stays in your blood longer, forcing your pancreas to release more insulin. Over time, this constant insulin release leads to insulin resistance and fat accumulation, especially around the waistline.
2. Lack of Movement After Meals
Many of us eat lunch at our desks and immediately jump into meetings or calls. When you don’t move after eating, your body doesn’t get a chance to use the glucose from your meal. Instead of being used as fuel, that glucose just keeps circulating in your bloodstream and again increasing insulin levels. A simple 10-minute walk post-lunch can make a huge difference in blood sugar balance.
3. Too Much Screen Time
Sitting in front of screens all day exposes you to blue light, which not only strains your eyes but also affects your circadian rhythm which is known as your body’s internal clock that regulates hormones, sleep and metabolism. Disrupted circadian rhythms can make your body less sensitive to insulin and increase sugar cravings, especially at night.
4. Stress Overload
Deadlines, work pressure, and constant multitasking keep your stress hormone (cortisol) elevated. High cortisol levels trigger the liver to release more glucose into your bloodstream, preparing your body for “fight or flight.” But since you’re sitting and not actually moving, that glucose just stays there, contributing again to insulin resistance. Chronic stress can also mess with hunger hormones, making you crave sugary or salty comfort foods.
5. Lack of Sunlight and Vitamin D Deficiency
Office jobs often mean spending most of the day indoors. But sunlight is your body’s natural source of vitamin D, which plays a key role in insulin sensitivity. Low vitamin D levels have been linked to poor blood sugar control and a higher chance of developing Type 2 Diabetes.
In short:
A desk job doesn’t directly cause insulin resistance, but the habits that come with it do. Sitting too long, skipping movement, staying stressed and eating irregularly slowly teach your body to stop responding properly to insulin.
Early Signs Your Body Might Be Insulin Resistant
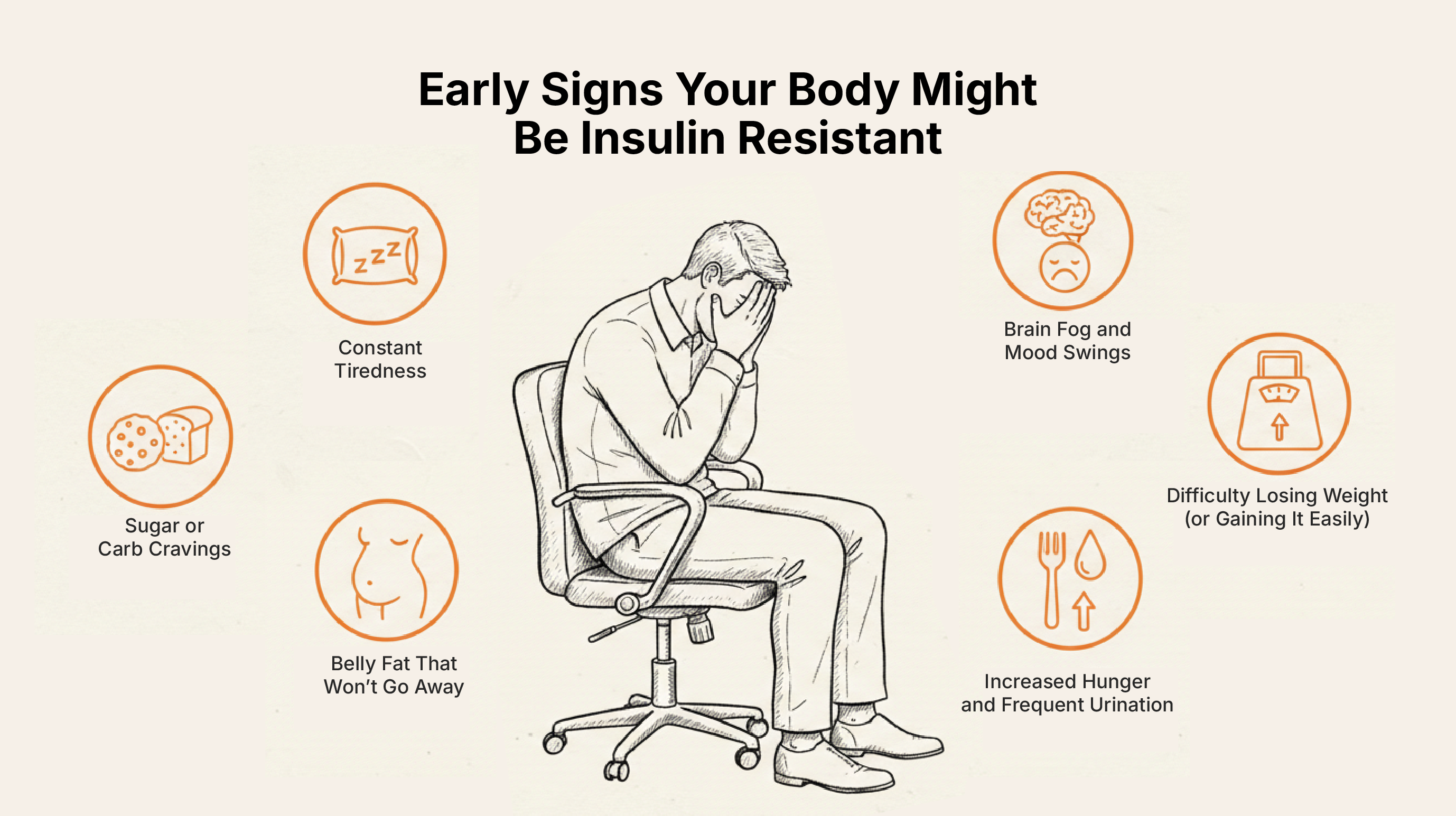
Here are some common early signs your body might be becoming insulin-resistant:
1. Constant Tiredness
You wake up tired, feel low on energy throughout the day and often need caffeine or sugar to “wake up.” That’s because your cells aren’t using glucose efficiently for energy, even though it’s there in your blood.
2. Belly Fat That Won’t Go Away
No matter how much you diet or exercise, fat seems to gather around your waist. When the insulin levels are high, your body starts storing more fat, especially around the abdominal area.
3. Sugar or Carb Cravings
You might find yourself craving sweets, biscuits, tea with extra sugar or evening snacks regularly. That’s because your body wants quick energy as your cells aren’t getting enough fuel from glucose.
4. Difficulty Losing Weight (or Gaining It Easily)
When insulin levels are high, your body switches into fat-storage mode. That makes it harder to lose weight and easier to gain it back, even if you eat healthy.
5. Brain Fog and Mood Swings
Unstable blood sugar can affect your mood, memory and focus. You might feel irritable, anxious or find it hard to concentrate, especially in the afternoon.
6. Increased Hunger and Frequent Urination
If you feel hungry soon after eating or need to use the washroom often, it might be your body’s way of signaling that your blood sugar isn’t being used properly.
7. Skin Changes
Dark, velvety patches on your neck, underarms or elbows (called acanthosis nigricans) can be an early physical sign of insulin resistance.
How to Manage Insulin Resistance
Your body has an incredible ability to heal and restore balance once you start treating it right. You don’t need drastic diets or long gym hours but you just need small, consistent changes that fit into your daily routine.
Here’s how you can start:
1. Move More Even While You Work
- Stand up every 30-45 minutes for a quick stretch or short walk.
- Take the stairs instead of the lift.
- Try walking calls or “desk stretches.”
- A 10-minute walk after meals helps your muscles use glucose better and keeps blood sugar levels stable.
2. Balance Your Plate
Your meals play a big role in improving insulin sensitivity.
- Focus on whole, unprocessed foods like veggies, protein, good fats and complex carbohydrates. Start your meals with good quality proteins and then good amount of fiber with less carbs.
- Avoid sugary coffee, processed snacks and refined carbs.
- Always combine carbohydrates with protein or healthy fats (like nuts, ghee, or eggs) to slow sugar spikes.
- Don’t skip meals or eat late at night because it confuses your metabolism.
3. Manage Stress
Stress triggers cortisol, which increases blood sugar. Over time, this constant stress response keeps your insulin levels high.
- Practice 5 minutes of deep breathing between meetings.
- Listen to calming music, meditate or simply sit in silence.
- Step outside during lunch to soak up some sunlight and breathe fresh air.
4. Prioritize Sleep
- Aim for 7–8 hours of restful sleep every night.
- Keep gadgets away at least 30 minutes before bed.
- Try maintaining a fixed sleep schedule
5. Get Your Sunlight and Vitamin D
- A few minutes of morning sunlight can naturally boost your vitamin D levels, improving your insulin sensitivity and mood.
- If your job keeps you indoors, get your vitamin D levels tested and supplement if needed.
6. Health Analysis
Sometimes, the only way to know what’s going on inside your body is through testing. A simple Root Cause Analysis (RCA) test from iThrive can help you check how your body is doing and if it needs any extra support. Knowing your numbers early can help you take the right steps before things go out of hand.
7. Support Your Body with the Right Supplements
Supplements can play a supportive role in improving insulin sensitivity, especially when combined with the right diet and lifestyle.
- Magnesium: improves sleep quality, giving your body the rest it needs
- Omega-3: Reduces inflammation that interferes with insulin signaling.
- Vitamin D3 K2: Supports glucose metabolism and overall energy.
Know how to build your own supplement stack click here

Subscribe to our newsletter and receive a selection of cool articles every week



.png)


.webp)

.jpg)
.jpg)