Introduction
Most people believe obesity begins when weight visibly increases. Clinically, it is often “diagnosed” when BMI crosses a cutoff or when clothes no longer fit the same way. But by the time this happens, the biological processes driving obesity have usually been active for years, and sometimes even decades.
At iThrive Alive, we do not view obesity as a sudden accumulation of fat. We see it as the final visible outcome of long-standing metabolic strain, hormonal compensation, and inflammatory signalling. Long before fat mass increases, the blood quietly records the body’s survival decisions.
These early changes don’t show up in routine check-ups focused only on fasting glucose or cholesterol totals. They appear in specific blood markers that reflect how the body is adapting to stress, energy excess, inflammation, and disrupted signalling. When interpreted correctly, these biomarkers can predict obesity risk well before weight gain begins.
This blog explains which blood markers predict obesity, why they change early, and how Alive uses them to intervene upstream, before the scale moves.
Why Weight Gain Is a Late Symptom, Not the Starting Point
Obesity is often framed as a failure of willpower. Biologically, it is anything but. The human body prioritises survival over aesthetics. When faced with repeated metabolic stress such as overnutrition, poor sleep, inflammation, emotional strain, toxin exposure, it eventually adapts.
Fat tissue expands not as excess, but as insurance:
- to store energy safely,
- to buffer inflammatory load,
- to protect vital organs from metabolic overflow.
This adaptive phase is invisible on the weighing scale. What is visible, however, is the blood. Hormones rise, inflammatory signals increase, lipid handling shifts, and insulin demand climbs. These changes precede weight gain and form the true early signs of obesity in blood tests.
This reframing is central to how Alive approaches obesity science: weight gain is not the cause, it is rather the consequence.
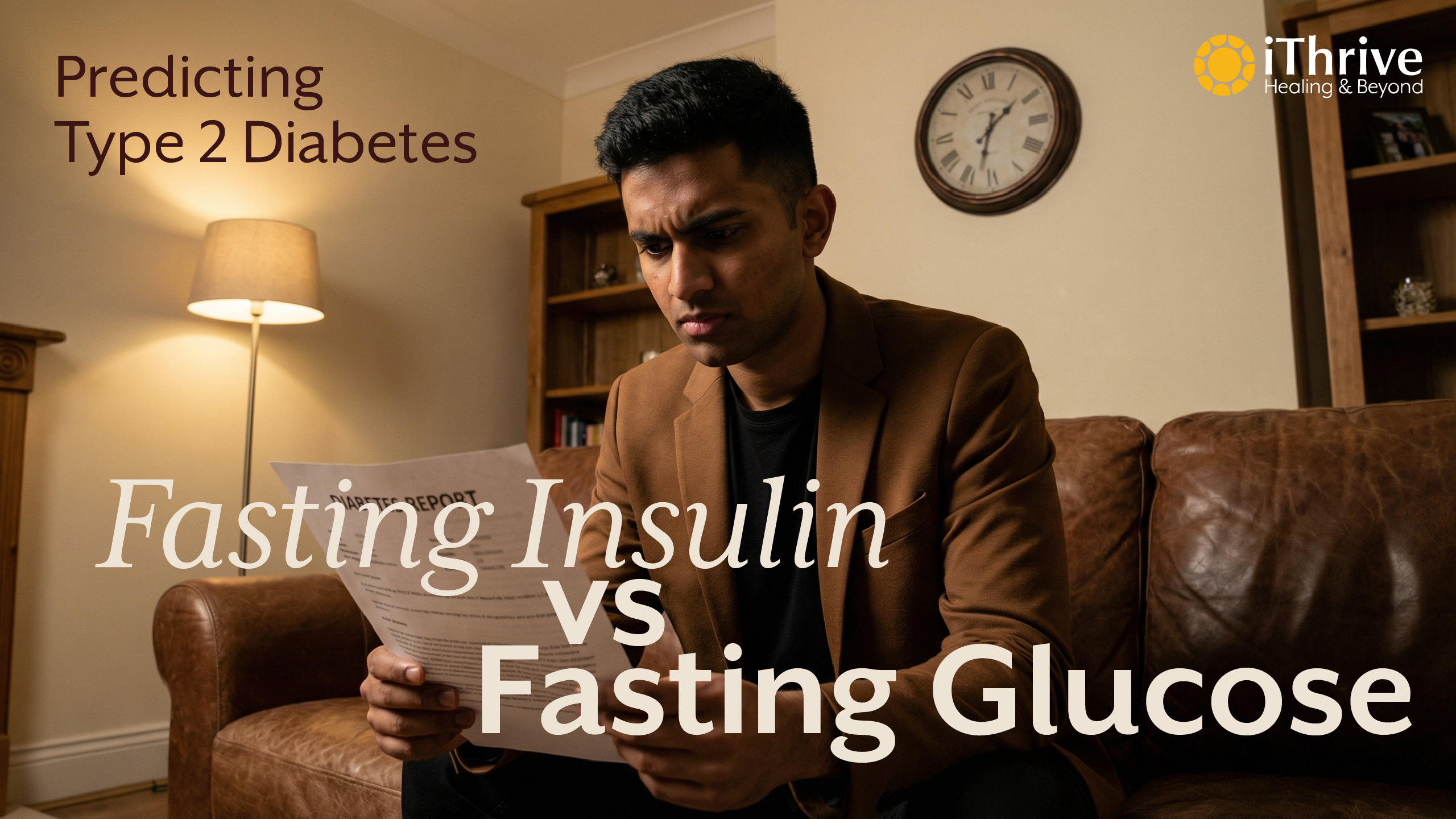
Fasting Insulin - The Earliest Obesity Risk Blood Marker
Fasting insulin is one of the most underutilised yet powerful biomarkers of obesity risk. While glucose reflects the result of regulation, insulin reflects the effort required to maintain that regulation.
When cells begin responding poorly to insulin, the pancreas compensates by producing more. Blood glucose may remain normal, but insulin rises quietly. This state, that is hyperinsulinemia, is not benign. It actively promotes fat storage and suppresses fat release.
Elevated fasting insulin years before weight gain signals:
- early insulin resistance,
- increased fat storage signalling,
- reduced metabolic flexibility.
Alive’s earlier blog on hyperinsulinemia as a hidden driver of metabolic disease explores how this state often exists undetected in “healthy” individuals. In obesity prediction, fasting insulin is foundational.
Inflammatory Markers - When Survival Mode Turns Chronic
Low-grade, chronic inflammation is a consistent predictor of future obesity. Markers such as high-sensitivity CRP (hs-CRP) often rise well before fat mass increases.
Inflammation alters insulin signalling, disrupts appetite regulation, and encourages fat storage as a protective buffer. Importantly, this is not acute illness inflammation, rather it is metabolic inflammation driven by:
- visceral fat signalling,
- gut barrier dysfunction,
- chronic stress physiology.
At Alive, inflammation is never viewed in isolation. We map it alongside insulin, lipid patterns, and lifestyle context to understand why the body has entered a defensive state.
Lipid Ratios - When Fat Handling Goes Wrong
Standard lipid panels often miss early obesity risk because totals can look “normal.” The real signal lies in patterns, especially:
- Elevated triglycerides
- Low HDL cholesterol
A rising triglyceride-to-HDL ratio reflects impaired fat oxidation and insulin resistance. It signals that the body is struggling to clear circulating energy efficiently and is redirecting it toward storage.
This lipid dysregulation is an early obesity blood marker, not merely a cardiovascular one.
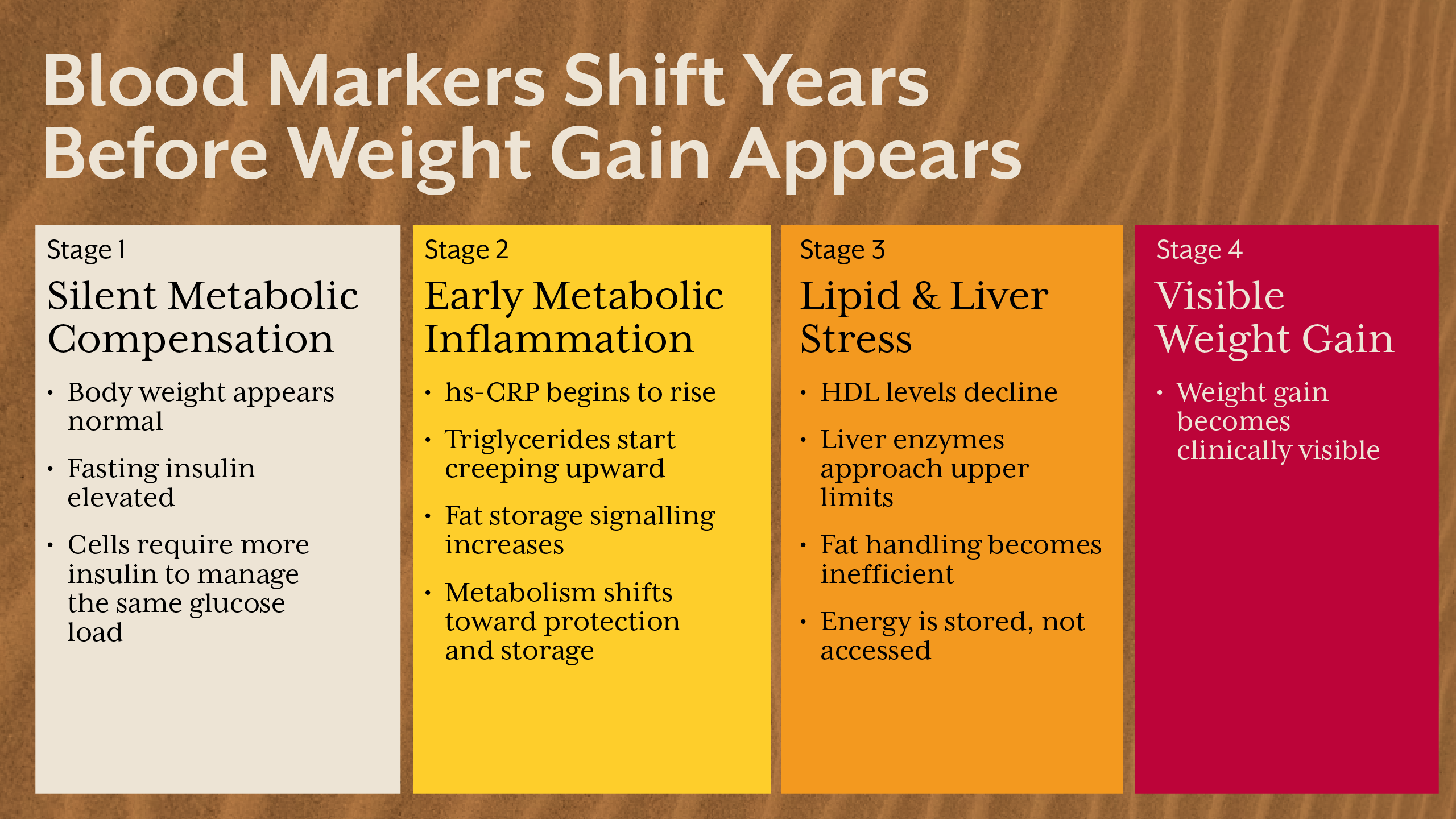
Liver Enzymes - The Silent Metabolic Alarm
Mild elevations in ALT and AST, even within “normal” ranges, often reflect early fat accumulation in the liver. Non-alcoholic fatty liver disease is not a consequence of obesity, it is frequently a precursor.
The liver governs glucose output, fat metabolism, and insulin clearance. When liver cells accumulate fat, insulin resistance accelerates system-wide.
Alive often sees liver markers shift long before individuals consider themselves overweight.
Leptin - When Satiety Signalling Breaks Down
Leptin is often called the “satiety hormone,” but its dysfunction is deeply misunderstood. Rising leptin levels indicate that the brain is no longer responding appropriately to fullness signals.
Leptin resistance develops early in metabolic dysfunction and contributes to:
- persistent hunger,
- reduced energy expenditure,
- defensive fat storage.
High leptin is not a lack of discipline, it is rather a communication failure between fat tissue and the brain.
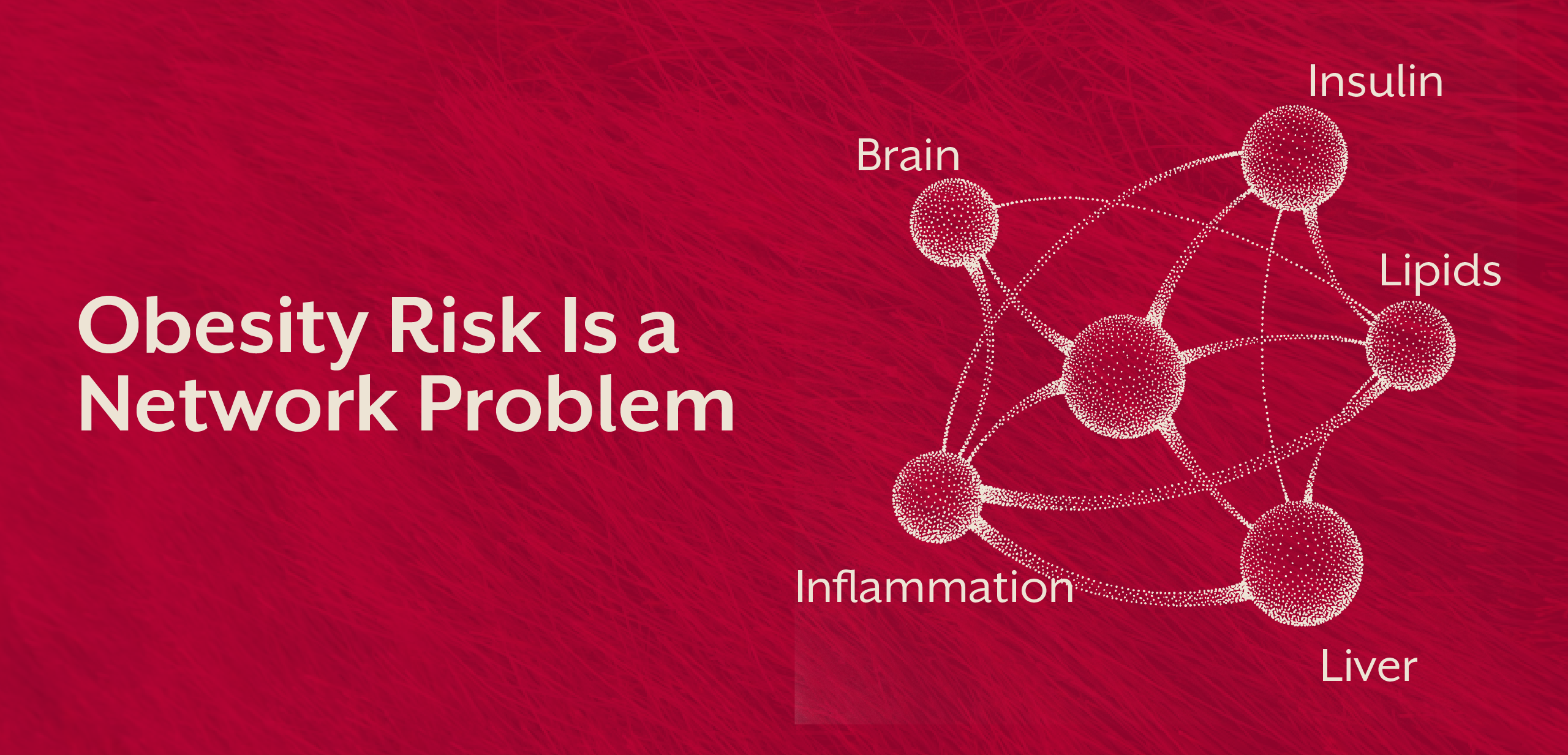
Why Single Tests Fail - Pattern Recognition Matters
No single blood test predicts obesity in isolation. The power lies in patterns across systems:
- insulin demand,
- inflammation,
- lipid handling,
- liver stress,
- appetite signalling.
This pattern-based interpretation is core to Alive’s root-cause analysis approach. Rather than asking “Is this value abnormal?”, we ask “What survival adaptation is this value reflecting?”
From Prediction to Prevention - What Changes the Trajectory
Identifying obesity risk blood markers is not about labelling disease—it is about timing intervention correctly. When addressed early, metabolic adaptations are reversible.
Alive focuses on:
- Restoring insulin sensitivity,
- Lowering inflammatory load,
- Improving liver fat handling,
- Re-establishing hormonal communication.
This is achieved through lifestyle alignment, smart supplementation, and signal-based eating, not calorie obsession. For individuals unsure which marker is driving their pattern, a structured root-cause clinical review helps identify the dominant lever.
Key Takeaway
Obesity does not appear suddenly, and it does not begin with weight gain. It begins as a series of quiet biochemical adaptations visible in blood long before the mirror reflects change. Fasting insulin, inflammatory markers, lipid ratios, liver enzymes, and hormonal signals together tell a story of a body trying to survive modern stressors. When these markers are interpreted early and in context, obesity becomes predictable, and more importantly, preventable. At iThrive Alive, this shift from reacting to weight gain toward understanding metabolic signals is what allows meaningful, lasting reversal rather than temporary weight loss.
Subscribe to our newsletter and receive a selection of cool articles every week



.png)


.webp)

.jpg)
.jpg)