Introduction
For decades, obesity has been framed as a personal failure like too much food, too little discipline, not enough movement. This narrative has shaped public health messaging, diet culture, and even clinical conversations. Yet despite an explosion of calorie-tracking apps, fitness programs, and “fat-loss hacks,” obesity rates continue to rise globally. If willpower were the real issue, this problem should have been solved by now.
At iThrive Alive, we approach obesity differently. We don’t see excess weight as a moral flaw or a lack of effort. We see it as a survival response, rather as a biological adaptation to internal chaos. When the body perceives threat, instability, or energy insecurity, it does what it has always done throughout human history: it stores.
To understand obesity properly, we must move away from blame and toward biology. This blog explores obesity science through the lens of metabolism, insulin signaling, inflammation, and evolutionary survival. More importantly, it explains why obesity is not about willpower, and why lasting change only occurs when root causes are addressed.
Obesity Explained Beyond Calories
Obesity vs Weight Loss Thinking
Weight loss focuses on the scale. Obesity science focuses on why the scale changed in the first place. Obesity is not simply excess fat mass; it is a state of metabolic dysfunction where the body has lost flexibility in how it uses and stores energy.
From a biological standpoint, obesity reflects:
- Chronic insulin elevation
- Impaired fat oxidation
- Inflammatory signaling
- Altered hunger and satiety hormones
This is why two people can eat similar diets and live similar lifestyles yet experience drastically different weight outcomes. Obesity causes are not uniform; they are deeply individual and metabolically driven.
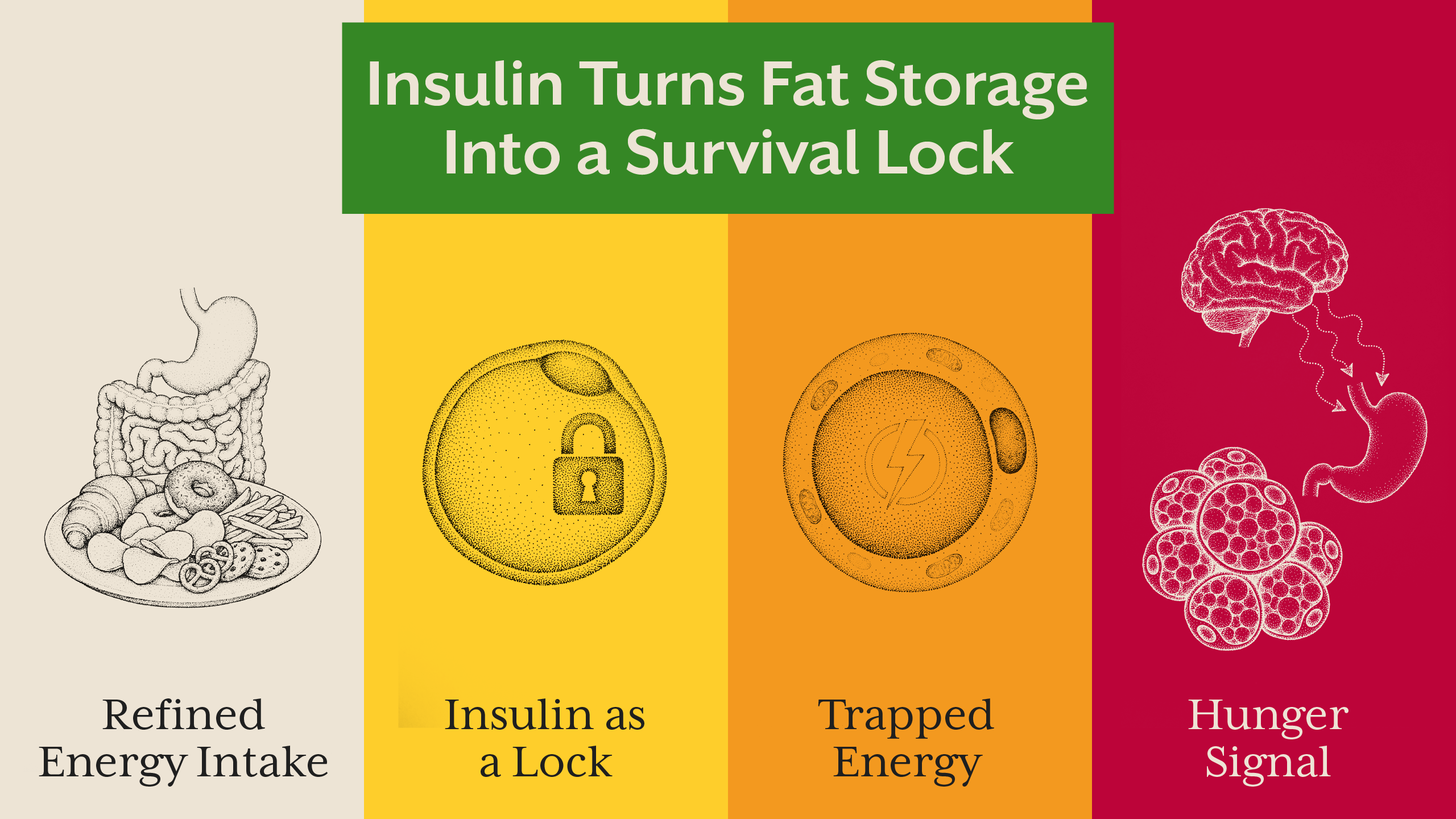
When obesity is reduced to “eat less, move more,” we ignore the fact that metabolism adapts. Calorie restriction without metabolic repair often worsens the problem by increasing stress hormones, slowing energy expenditure, and reinforcing fat storage.
Obesity and Metabolism - The Survival Switch
The Body Under Threat
The human body evolved to survive scarcity, infection, and environmental stress. When modern stressors like processed food, sleep disruption, chronic inflammation, toxins, emotional strain mimic these threats, the body responds in the same way it always has: by conserving energy.
Insulin plays a central role here. Chronically elevated insulin acts as a metabolic lock, preventing fat breakdown and signaling the body to store incoming energy. This state is often present years before diabetes is diagnosed, a concept explored in our blog “Hyperinsulinemia: The Hidden Driver of Metabolic Disease” on Alive.
Importantly, obesity is often a protective adaptation, not a malfunction. Fat tissue acts as:
- A buffer for excess glucose
- A storage site for inflammatory byproducts
- A hormonal signaling organ
From a survival perspective, this makes sense. From a modern health perspective, it becomes problematic.
Why Obesity Is Not About Willpower
The Neurobiology of Eating
Willpower assumes conscious control. Obesity science shows that most eating behavior is hormonally driven. Insulin, leptin, ghrelin, cortisol, and dopamine shape hunger, cravings, and satiety long before conscious thought enters the picture.
When insulin remains high:
- Leptin signaling becomes impaired
- The brain perceives energy deficiency
- Hunger persists despite adequate fat stores
This is why individuals with obesity are often biologically hungrier, not weaker. Blaming willpower ignores the neurological reality of metabolic disease.
At iThrive Alive, we frequently see individuals who have tried “everything” such as clean eating, intermittent fasting, intense workouts yet remain stuck. When we correct insulin signaling, gut health, micronutrient deficiencies, and circadian rhythm, hunger normalizes without force.
This reframing is central to obesity myths versus obesity science.
Root Causes Behind the Obesity Problem
Looking Beneath the Surface
Obesity causes rarely exist in isolation. At Alive, root cause analysis often reveals overlapping contributors:
- Gut dysbiosis and endotoxin load
- Chronic low-grade inflammation
- Sleep fragmentation and cortisol excess
- Micronutrient depletion
- Ancestral and epigenetic programming
This is why obesity often coexists with PCOS, fatty liver, insulin resistance, and thyroid dysfunction. Treating weight alone misses the broader metabolic picture.
Our approach mirrors what we discussed in “Insulin Resistance: The Silent Phase Before Disease” long before lab values cross diagnostic thresholds, the body is compensating.
The iThrive Alive Approach to Obesity Reversal
Food as Biological Signaling
At iThrive Alive, obesity reversal is not about dieting, it’s about changing the signal. Through lifestyle interventions, smart supplementation, and precise food sequencing, we restore metabolic flexibility.
Key principles include:
- Reducing insulin spikes through meal composition and order
- Prioritizing bioavailable protein
- Removing inflammatory seed oils
- Supporting insulin sensitivity with targeted micronutrients
- Aligning eating patterns with circadian biology
This approach is deeply individual. That’s why root cause assessment remains foundational. For those seeking structured guidance, a clinical review helps identify which systems are driving weight retention.

Key Takeaway
Obesity is not a personal failure, rather is a biological response to sustained metabolic stress. When the body perceives instability, it stores energy as protection. Lasting change occurs only when this perceived threat is removed. By addressing insulin signaling, inflammation, gut health, sleep, and nutrient status, the body no longer needs excess weight for survival. True obesity reversal is not forced; it is allowed.
Subscribe to our newsletter and receive a selection of cool articles every week



.png)


.webp)

.jpg)
.jpg)