Introduction
Type 2 diabetes is often described as a lifelong condition that needs constant “management.” Monitor sugar, take medication, adjust doses, repeat. For millions, this becomes the rhythm of daily life. Yet despite doing everything right on paper, many people still feel worse over time. Energy drops. Weight creeps up. Medications increase. Complications loom.
This raises an uncomfortable but necessary question. Are we truly treating the disease or are we only managing its most visible symptom?
To understand the real difference between managing diabetes and fixing metabolism, we need to move beyond blood sugar alone and look at insulin resistance, metabolic infrastructure, and the root cause of diabetes itself.
Managing Diabetes: The Conventional Approach
What “management” usually means
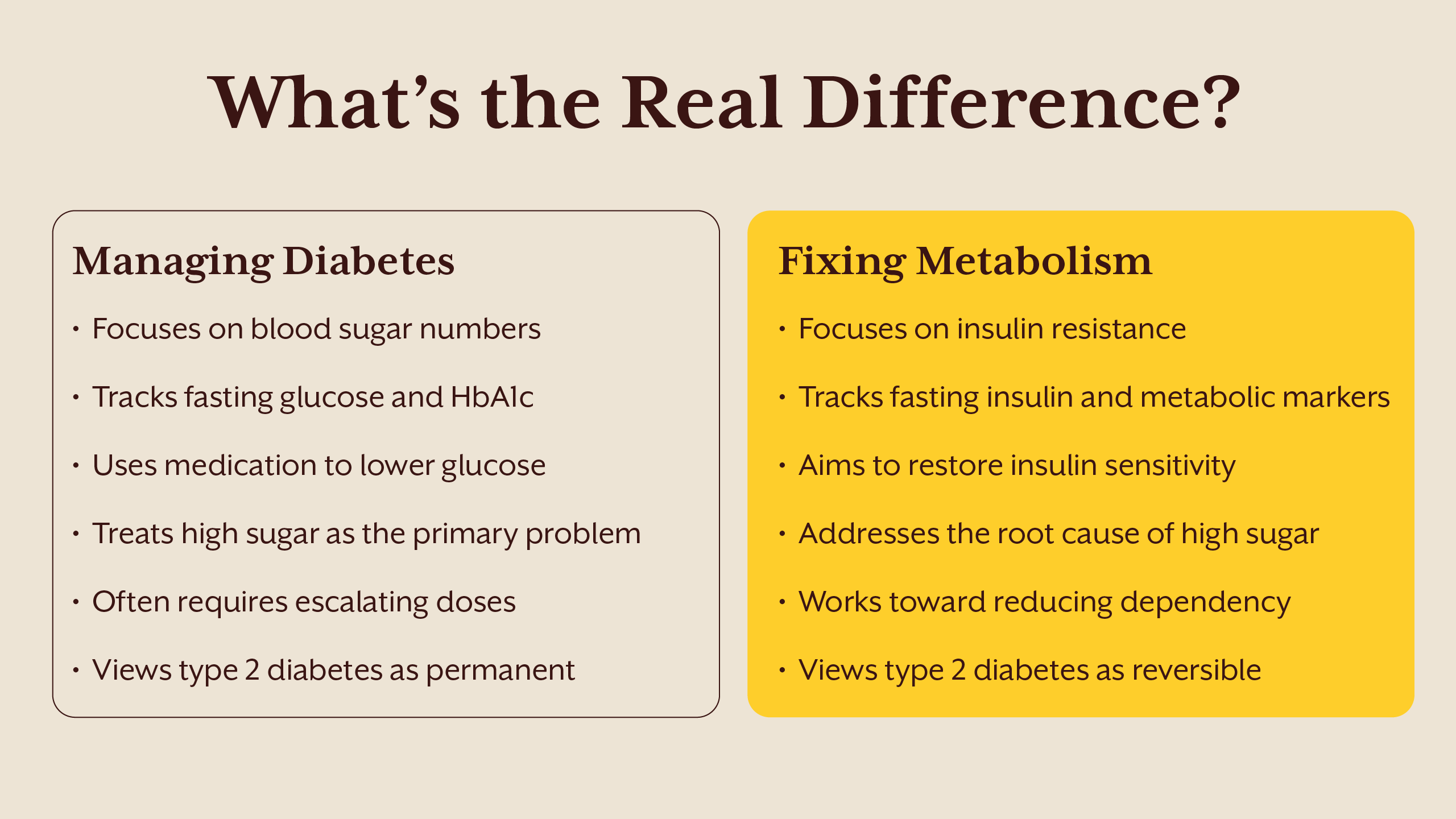
In conventional care, type 2 diabetes is primarily tracked using fasting glucose and HbA1c. If blood sugar is high, treatment is escalated. If numbers improve, the disease is considered controlled.
Medications play a central role. These may include drugs that increase insulin secretion, improve insulin sensitivity, reduce glucose absorption, or promote glucose loss through urine. Each has a defined mechanism and short term benefit.
On the surface, this approach makes sense. High blood sugar is dangerous, and lowering it reduces immediate risk.
If you are new to diabetes care and want a clearer understanding of standard treatment pathways, you can also read our blog on Diabetes Management for Beginners: A Guide to the Right Steps for a Healthier Life.
The limitation of glucose focused care
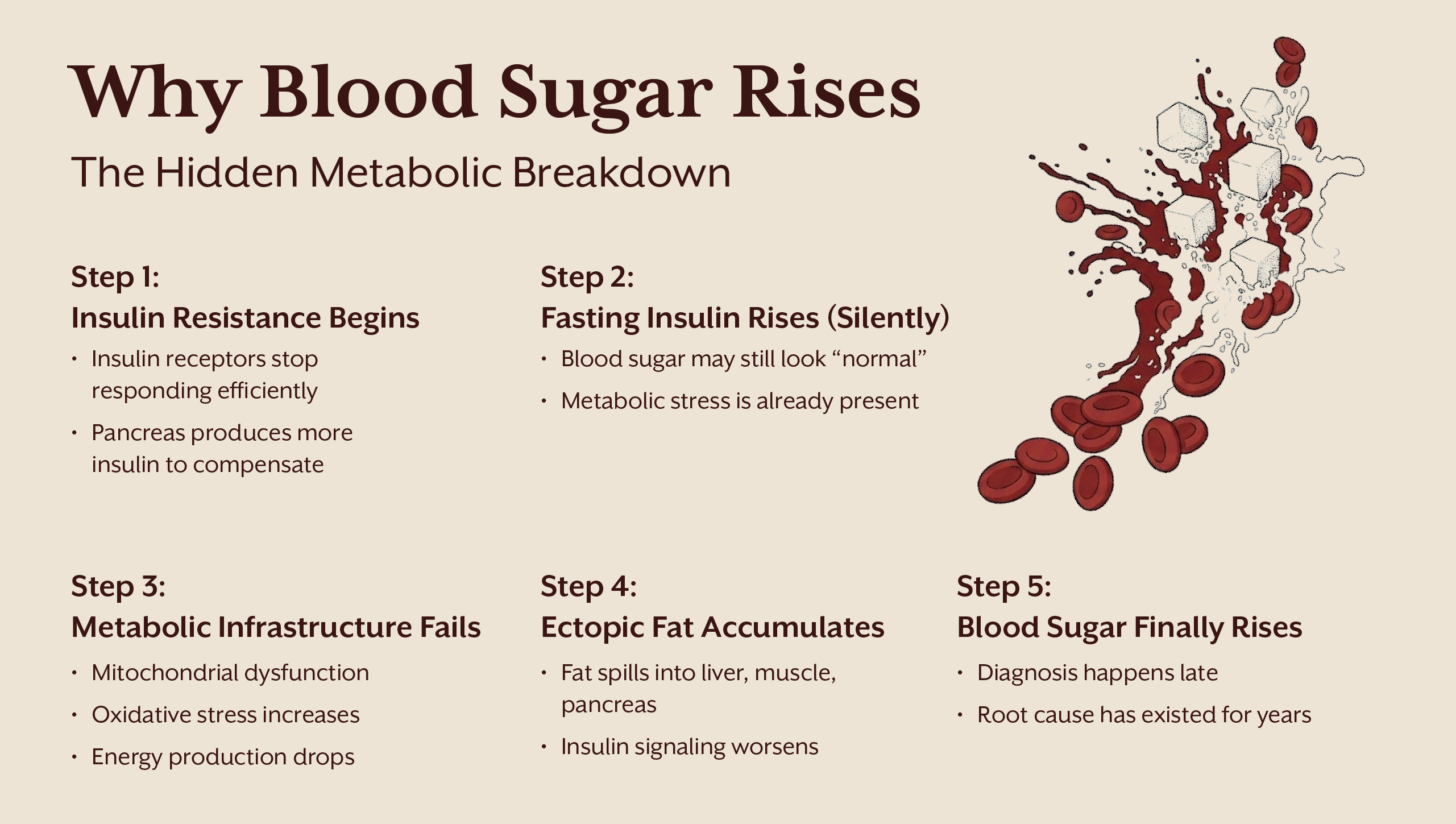
The problem is not that glucose doesn’t matters. The issue is that glucose is a lagging indicator. By the time fasting glucose or HbA1c rises, metabolic dysfunction has usually been present for years.
Insulin resistance often precedes type 2 diabetes by a decade or more. During this phase, insulin levels climb to keep blood sugar normal. Lab reports may still look fine, yet the body is already under strain.
When treatment focuses only on lowering sugar without addressing insulin resistance, it is similar to silencing a fire alarm without putting out the fire. The alarm stops, but the damage continues quietly.
Insulin Resistance: The Hidden Driver
What insulin resistance actually is
Insulin resistance is not a single organ problem. It is a systems level breakdown involving the liver, muscle, adipose tissue, mitochondria, and hormonal signaling.
In muscle, insulin resistance reduces glucose uptake due to impaired GLUT4 translocation. In the liver, insulin fails to suppress glucose production, leading to elevated fasting and post meal sugars. In adipose tissue, dysfunctional fat cells release inflammatory signals and excess fatty acids into circulation.
This creates a state where the body must produce more and more insulin just to maintain balance.
Fasting insulin reveals what glucose hides
One of the most overlooked markers in diabetes care is fasting insulin. While fasting glucose tells you how much sugar is in the blood, fasting insulin tells you how hard the body is working to keep it there.
A normal fasting glucose with elevated fasting insulin signals metabolic stress. It means the pancreas is compensating aggressively. This is often the earliest measurable sign of insulin resistance and one of the clearest windows into the root cause of diabetes.
Ignoring fasting insulin means missing the disease in its most reversible stage.
The Metabolic Infrastructure Problem
Mitochondria, oxidative stress, and energy failure
At the cellular level, insulin resistance is closely tied to mitochondrial dysfunction. Excess nutrient load, oxidative stress, endotoxins, and chronic inflammation impair oxidative phosphorylation. ATP production falls. Reactive oxygen species rise.
As mitochondrial efficiency drops, insulin signaling pathways become disrupted. Cells struggle to process glucose and fat efficiently. This metabolic inflexibility forces the body into survival mode rather than repair mode.
Blood sugar rises not because the body is broken, but because it is overwhelmed.
Ectopic fat and metabolic congestion
When adipose tissue storage capacity is exceeded, fat spills into organs not designed to store it. Liver, muscle, pancreas. This ectopic fat interferes with insulin signaling through lipid intermediates such as ceramides and diacylglycerols.
In the pancreas, fat accumulation impairs beta cell function. In the liver, it drives excess glucose production. This is the biological basis of the twin cycle hypothesis and a central piece of the root cause of diabetes.
Ectopic fat and metabolic congestion
When adipose tissue storage capacity is exceeded, fat spills into organs not designed to store it. Liver, muscle, pancreas. This ectopic fat interferes with insulin signaling through lipid intermediates such as ceramides and diacylglycerols.
In the pancreas, fat accumulation impairs beta cell function. In the liver, it drives excess glucose production. This is the biological basis of the twin cycle hypothesis and a central piece of the root cause of diabetes.
Fixing Metabolism: A Root Cause Strategy
What fixing metabolism actually means
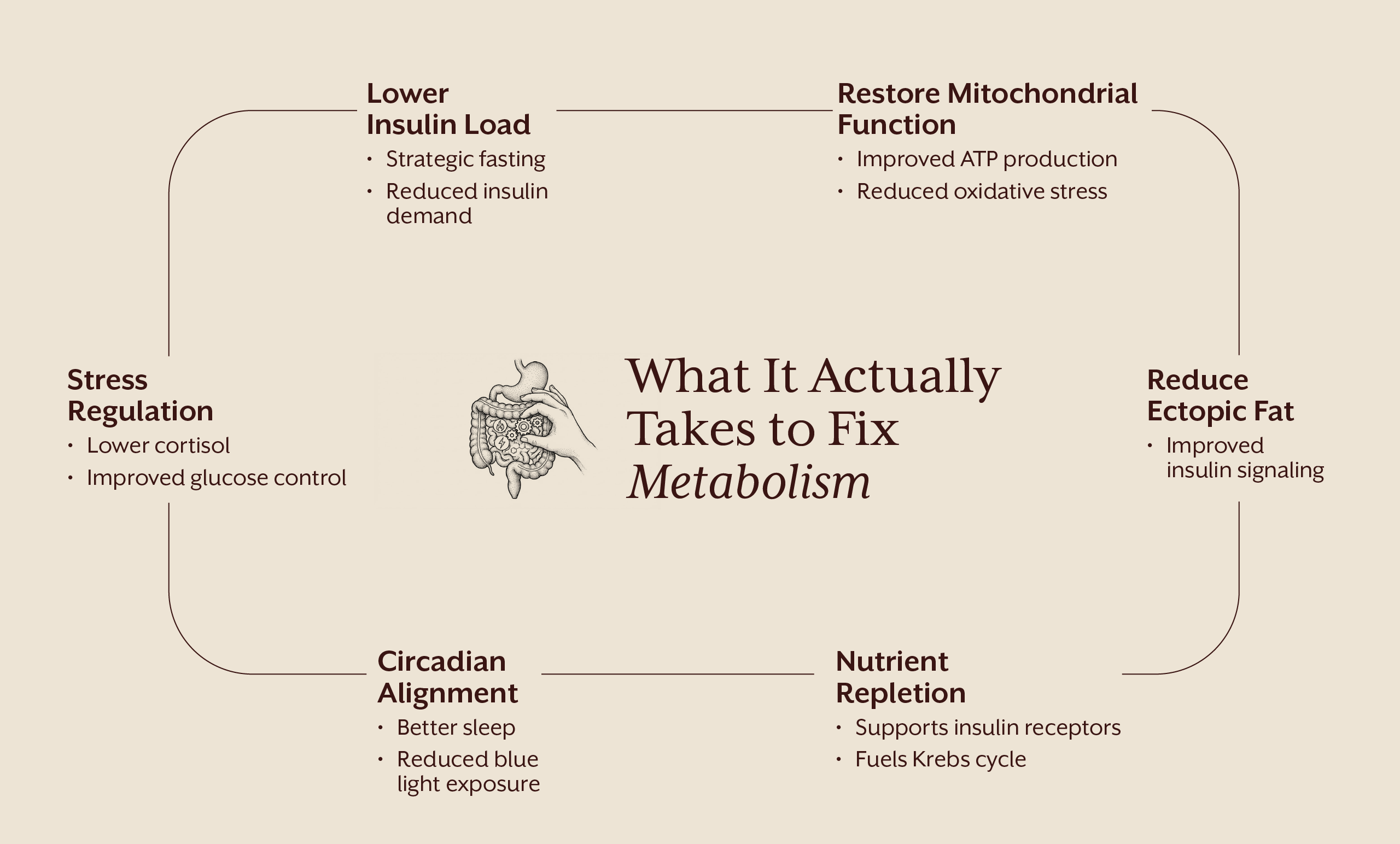
Fixing metabolism is not about chasing numbers. It is about restoring physiological responsiveness. When metabolism works, insulin is released appropriately, receptors respond efficiently, mitochondria produce energy cleanly, and glucose returns to cells without force.
This approach views type 2 diabetes as a potentially reversible state of metabolic dysfunction, not an irreversible disease.
For those questioning whether type 2 diabetes can truly be reversed rather than managed, our blog Reversing Diabetes Is Possible: Here’s How.. dives deeper into the practical application of this approach.
The role of fasting and fasting insulin
Strategic fasting, when appropriate and personalized, reduces insulin levels and allows receptors to resensitize. Lower insulin enables fat mobilization, reduces ectopic fat, and improves mitochondrial efficiency.
Tracking fasting insulin alongside glucose provides feedback on whether the intervention is working at the root level, not just cosmetically.
Fasting is not a tool of deprivation. It is a biological signal that allows the body to switch from constant storage to repair and cleanup.
Nutrients and the Cellular Engine
The overlooked role of micronutrients
Insulin signaling depends on key nutrients such as magnesium, chromium, zinc, and B vitamins involved in the Krebs cycle. Deficiencies impair glucose metabolism even when diet appears adequate.
Without these cofactors, insulin receptors do not respond properly and mitochondria cannot generate energy efficiently. Supplementation in this context is not optional support. It is a foundational repair.
If you want to understand how food and targeted nutrition actively influence insulin signaling and cellular energy, explore our detailed breakdown in Fighting Diabetes with Food: The Science Behind Functional Nutrition.
Oxidative load and inflammation
Markers like hs CRP, ferritin, uric acid, and homocysteine reflect metabolic wear and tear. Elevated levels indicate oxidative stress and inflammation that directly worsen insulin resistance.
Reducing this load through nutrition, sleep, stress regulation, and targeted compounds improves metabolic signaling across tissues.
Managing vs Fixing: The Core Difference
Managing diabetes focuses on controlling outputs. Fixing metabolism focuses on repairing inputs.
Management asks, how do we lower blood sugar today? Fixing asks, why does blood sugar rise in the first place?
Management often leads to escalating medication. Fixing aims for reducing dependency over time.
Management treats type 2 diabetes as permanent. Fixing recognizes that biology responds when conditions change.
This is not anti-medicine. It is pro-physiology.
The iThrive Perspective
At iThrive Alive, the focus is not on suppressing symptoms but on rebuilding metabolic infrastructure. This means assessing insulin resistance directly, measuring fasting insulin, understanding nutrient status, evaluating stress and circadian alignment, and personalizing interventions. The goal is not perfection. It is progress toward resilience. For those seeking clarity on their metabolic state, understanding insulin resistance early can change the entire trajectory. You can book a free consult to explore whether your current approach is managing numbers or fixing metabolism.
Key Takeaways
Type 2 diabetes is not just a blood sugar problem. It is a deeper metabolic dysfunction that builds silently over time. Managing diabetes focuses on controlling glucose levels, while fixing metabolism addresses insulin resistance, the true root cause. Fasting insulin often reveals metabolic stress years before blood sugar levels rise, making it a powerful marker for early insight. Metabolic health depends on mitochondrial function, nutrient status, sleep, stress, and circadian rhythm, not willpower alone. Understanding whether you are managing numbers or repairing metabolism requires the right data. You can book a free consult to gain clarity on your metabolic health.
Subscribe to our newsletter and receive a selection of cool articles every week



.png)


.webp)

.jpg)


.webp)
.webp)