Introduction
For many individuals diagnosed with thyroid dysfunction, treatment begins and ends with medication. Hormone replacement or suppression can normalize laboratory values, but it does not always resolve persistent thyroid symptoms such as fatigue, weight changes, hair loss, brain fog, or temperature sensitivity. This gap between biochemical correction and physiological recovery is becoming increasingly recognized in clinical practice.
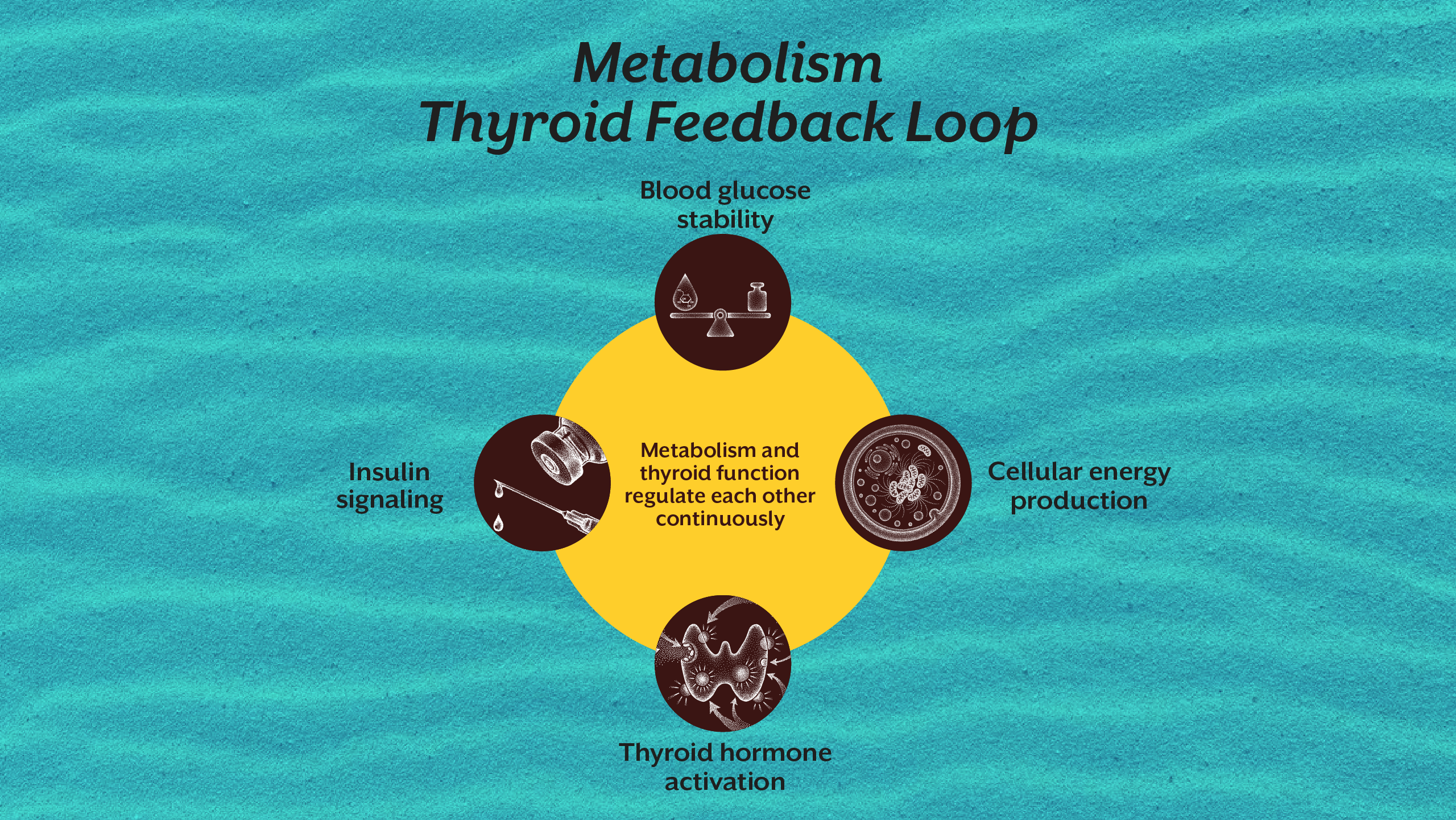
The thyroid gland does not function in isolation. Thyroid hormone function depends on nutrient availability, cellular energy production, immune stability, metabolic health, circadian rhythm integrity, and stress signaling. When these regulatory systems are disrupted, medication alone cannot fully restore thyroid physiology.
This explains why individuals with “normal thyroid levels” may continue to experience thyroid disease symptoms. It also explains why thyroid problems are rising globally, particularly among young adults and women. The issue is not simply hormone deficiency, it is regulatory dysfunction.
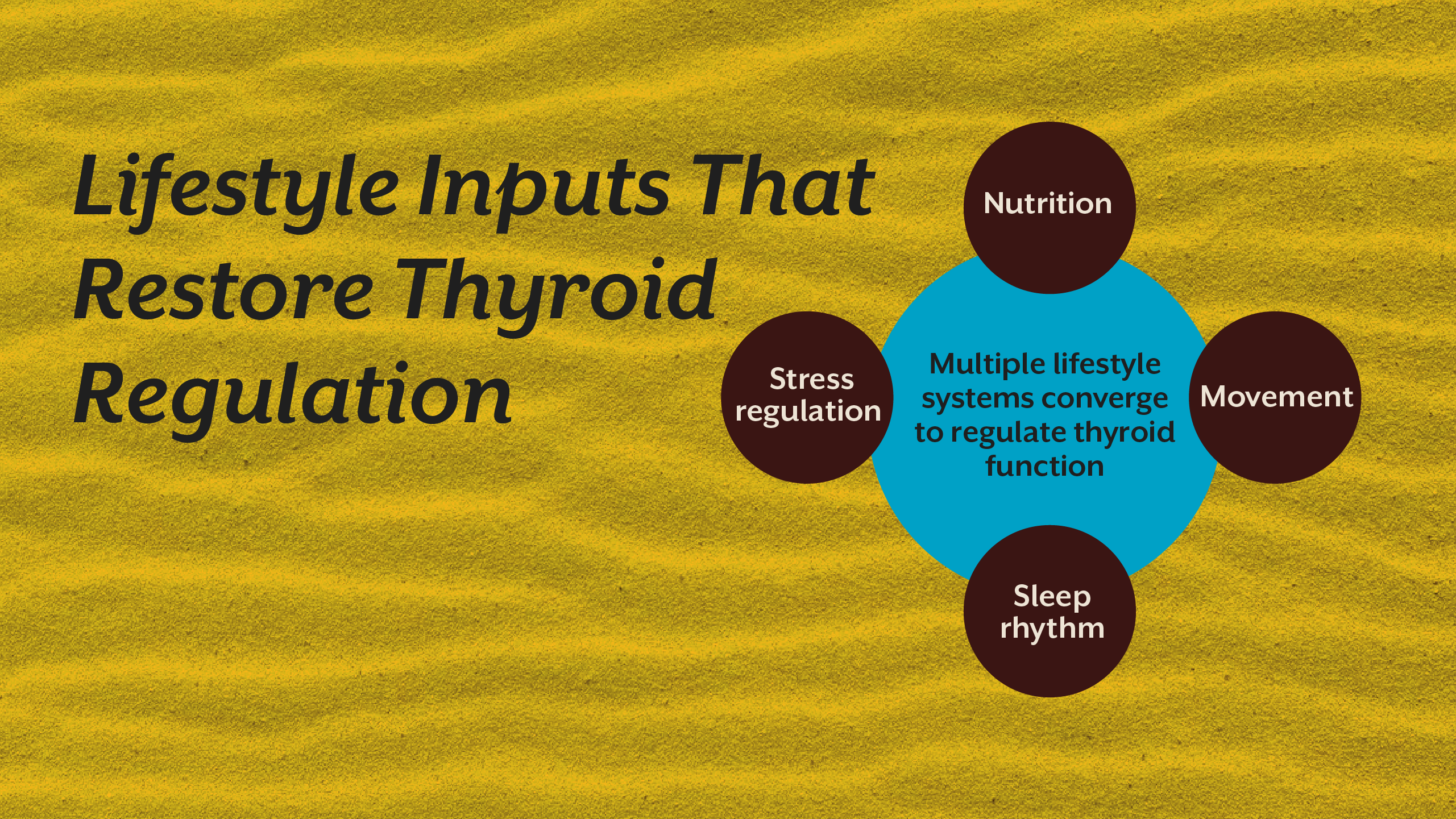
Lifestyle interventions influence the very mechanisms that determine how thyroid hormones are produced, converted, transported, and used by cells. Understanding these mechanisms transforms how we approach thyroid treatment. Instead of managing hormone levels alone, we begin restoring the biological environment that allows thyroid regulation to occur naturally.
This systems-based approach is central to clinical work at iThrive Alive, where thyroid physiology is evaluated as part of a broader metabolic and regulatory network rather than as an isolated endocrine problem.
Section 1 - Why Medication Alone Does Not Fully Restore Thyroid Health
Medication replaces or modifies hormone levels. But thyroid regulation is more complex than hormone presence in the bloodstream.
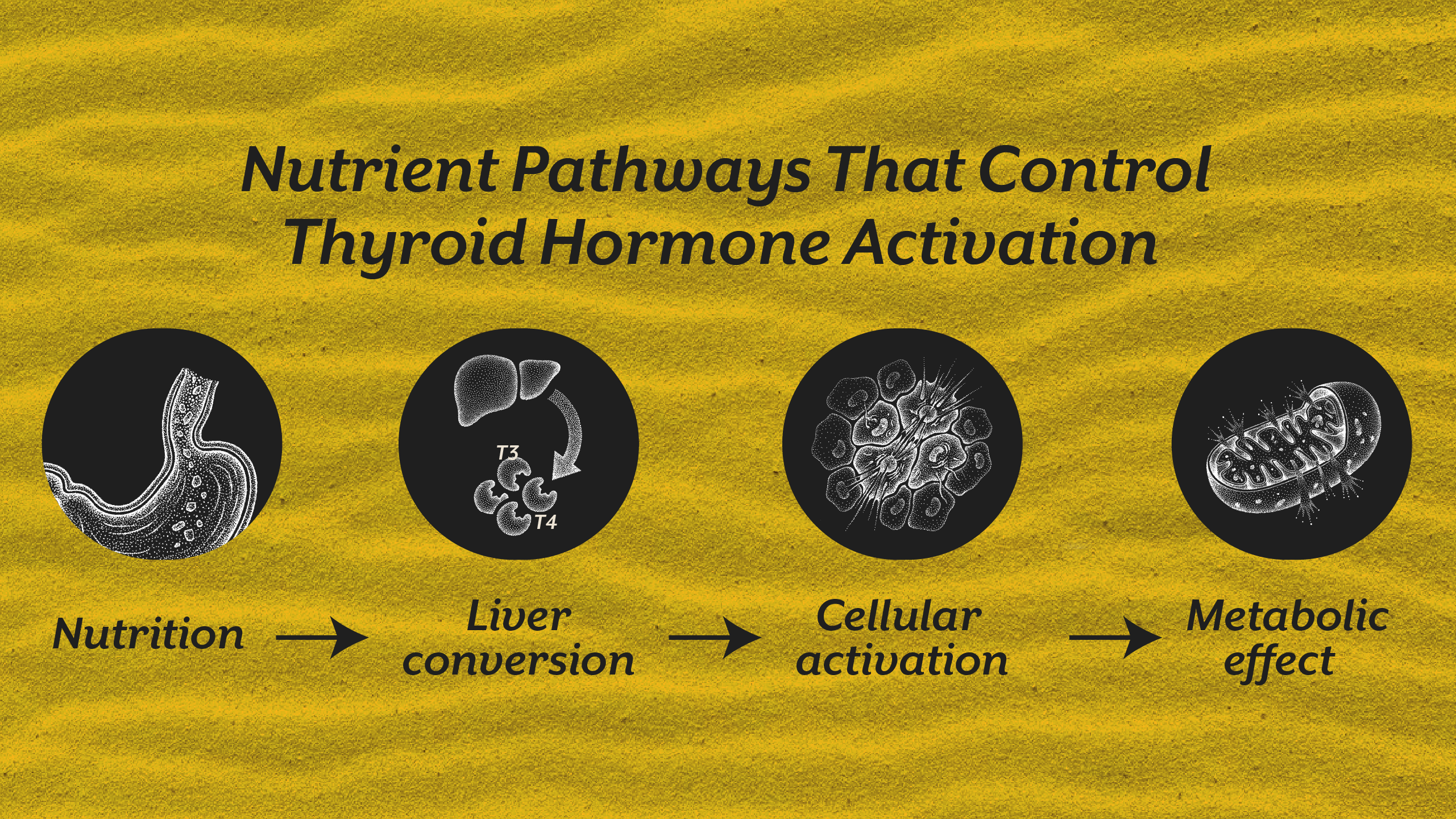
Thyroid hormones must be absorbed, converted, transported into cells, and activated at the mitochondrial level to produce metabolic effects. Disruption at any step can produce thyroid symptoms even when laboratory values appear normal.
Hormone Conversion Matters More Than Hormone Quantity
The most circulating thyroid hormone is T4, an inactive precursor. Cells require T3, the active form. Conversion depends on liver function, gut health, micronutrient sufficiency, and inflammatory load. When conversion is impaired, individuals may experience symptoms of hypothyroidism despite normal thyroid levels.
Cellular Responsiveness Determines Metabolic Impact
Hormone signaling depends on receptor sensitivity and mitochondrial energy production. Chronic stress, insulin resistance, and inflammation reduce cellular responsiveness, meaning hormones cannot exert full metabolic effects.
Regulatory Systems Influence Hormone Stability
Sleep quality, circadian rhythm, and nervous system balance influence hormone release patterns. Disrupted rhythms alter metabolic signaling and contribute to thyroid causes that standard treatment does not address.
Medication corrects hormone concentration. Lifestyle interventions restore regulatory function.
Section 2 - Nutritional Physiology and Thyroid Hormone Function
Nutrition influences thyroid health far beyond iodine intake. Hormone production, conversion, and cellular utilization depend on multiple nutrient-dependent pathways.
Micronutrient-Dependent Hormone Activation
Selenium supports T4 to T3 conversion. Zinc influences receptor binding. Iron supports thyroid enzyme activity. Deficiency in any of these alters hormone efficiency rather than hormone quantity.
Protein and Metabolic Signaling
Adequate protein intake supports hepatic hormone processing and stabilizes blood glucose. Metabolic instability disrupts thyroid signaling through stress hormone activation.
Inflammation-Modulating Nutrition
Chronic inflammatory signaling interferes with hormone conversion and increases reverse T3 production, a metabolically inactive form that slows cellular energy production.
For many individuals searching “diet for thyroid patients” or “best food for thyroid patients,” the relevant question is not simply what to eat, but what metabolic environment food creates.
Section 3 - Stress Physiology and Thyroid Regulation
Stress is one of the most underestimated thyroid causes. It directly alters hormone conversion, receptor sensitivity, and metabolic signaling.
Cortisol and Hormone Conversion
Elevated cortisol reduces T4 to T3 conversion and increases reverse T3 production. This slows metabolism and contributes to fatigue and weight gain.
Nervous System Dominance and Metabolic Suppression
Chronic sympathetic activation prioritizes survival over energy expenditure. The body conserves energy by reducing thyroid activity.
Sleep Disruption and Hormone Rhythm
Poor sleep alters hypothalamic-pituitary signaling, affecting hormone release timing and metabolic efficiency.
Individuals searching “how to control thyroid naturally” often overlook stress physiology as a primary regulatory factor.
Section 4 - Metabolic Health and Thyroid Regulation
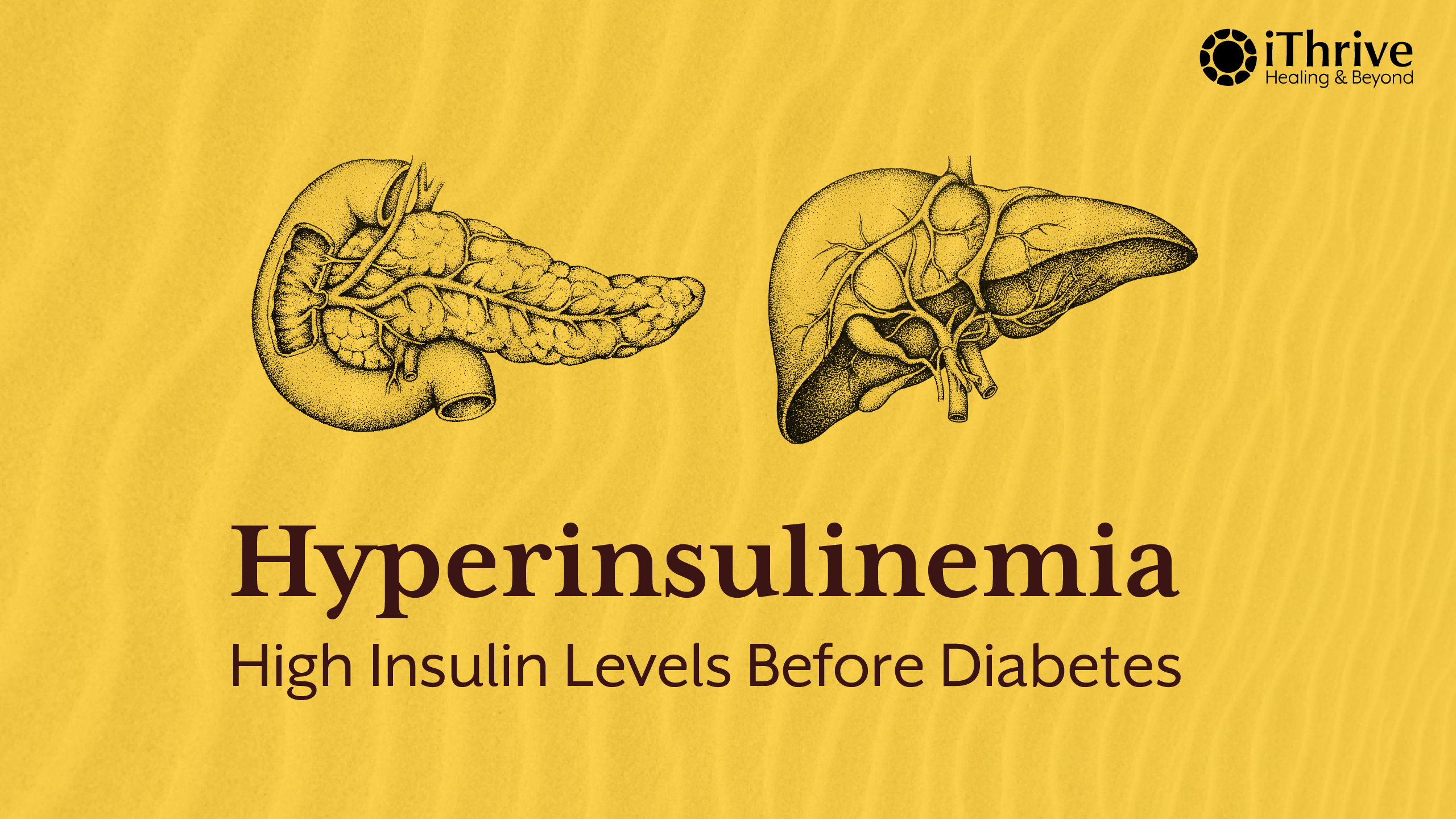
Thyroid function is tightly linked to metabolic health. Insulin resistance alters hormone transport and cellular energy availability.
When cells cannot effectively use glucose, metabolic signaling changes. The body reduces energy expenditure, which is reflected in altered thyroid hormone activity.
This connection explains why individuals with weight changes, fatigue, and hair loss often experience overlapping metabolic and thyroid disease symptoms.
Metabolic regulation is therefore a critical component of natural thyroid treatment.
Section 5 - Circadian Rhythm and Thyroid Function
Thyroid hormones follow daily rhythmic patterns. Light exposure, sleep timing, and meal timing influence hormone release and metabolic efficiency.
Circadian disruption alters endocrine communication between the brain and thyroid gland. Shift work, irregular sleep, and late-night eating interfere with this coordination.
Many individuals with persistent thyroid symptoms also show circadian misalignment, yet this remains rarely addressed in standard thyroid treatment.
Section 6 - Movement and Cellular Energy Production
Physical activity influences mitochondrial function, hormone receptor sensitivity, and metabolic flexibility. Sedentary behavior reduces cellular energy production and slows thyroid-mediated metabolism.
Resistance training, in particular, improves glucose utilization and enhances tissue responsiveness to thyroid hormones.
Movement therefore functions as a metabolic regulator rather than merely a calorie-burning tool.
Section 7 - Why Personalized Assessment Matters
No single lifestyle change restores thyroid function for everyone. Each individual’s regulatory imbalance differs like their nutrient deficiency, metabolic dysfunction, immune activation, or stress physiology.
This is why comprehensive evaluation is essential. Identifying specific drivers allows targeted lifestyle interventions rather than generalized advice.
Individuals seeking deeper understanding of persistent thyroid disease symptoms often choose to book a root cause analysis or book a consult to evaluate regulatory factors beyond hormone levels.
Section 8 - Integrating Lifestyle With Clinical Thyroid Care
Lifestyle interventions do not replace medication when clinically required. Instead, they enhance physiological responsiveness and improve long-term regulation.
This integrative perspective is explored in greater depth in:
• “Why Thyroid Disorders Are Rising: The Hidden Root Causes Conventional Testing Misses”
• “The Thyroid-Gut Axis: How Microbiome Imbalance Disrupts Hormone Conversion”
Together, these frameworks explain why natural treatment for thyroid must address regulatory networks rather than isolated hormone levels.
Key Takeaway
Thyroid regulation is not determined solely by the gland or by hormone concentration in blood tests. It emerges from the coordinated function of metabolic signaling, nutrient availability, stress physiology, circadian rhythm, immune balance, and cellular energy production. Medication can correct hormone levels, but it cannot independently restore the biological systems that regulate hormone activation and responsiveness. Sustainable thyroid health therefore requires a systems-level approach that integrates nutrition, sleep, stress regulation, metabolic stability, and personalized clinical evaluation. When these regulatory networks are supported, the body regains the capacity to maintain thyroid balance naturally rather than relying exclusively on external hormone control.
Subscribe to our newsletter and receive a selection of cool articles every week




.png)


.webp)

.jpg)
.jpg)