Modern weight management conversations often revolve around calories, discipline, and behavioral control. Yet clinical metabolic research increasingly reveals that appetite, fat storage, and energy expenditure are not merely behavioral outcomes, they are biologically regulated processes governed by cellular signaling networks.
Among the most powerful signaling molecules currently studied in metabolic medicine are therapeutic peptides. These short chains of amino acids function as highly specific biological messengers that instruct cells to modify metabolic activity, regulate appetite, influence energy utilization, and in some cases accelerate fat loss.
Unlike traditional metabolism boosters or appetite suppressants that act broadly across systems, therapeutic peptides operate through receptor-level communication. They do not simply stimulate or suppress, rather they inform. They alter how the body perceives energy sufficiency, nutrient availability, and metabolic demand.
This is precisely why peptides for weight loss are receiving increasing attention. However, at a clinical level, their role is far more nuanced than rapid fat reduction. They interact with insulin signaling, gut-brain communication, inflammatory pathways, and neuroendocrine regulation.
At iThrive, peptide therapy is never viewed as an isolated intervention. It is examined within the broader landscape of metabolic health, cellular repair, and root-cause physiology, the same systems discussed in our published articles “Hyperinsulinemia: Hidden Cause of Weight Gain and Diabetes” and “How I lost 16 kgs in 4 months - Mugdha Pradhan’s easy weight loss journey with GLP agonists.”
To understand why therapeutic peptides are powerful and why they must be used responsibly, we must first understand how they communicate within the body.
Cellular Communication: Why Peptides Influence Metabolism So Powerfully
The human body functions through layered communication systems. Hormones transmit broad systemic messages. Neurotransmitters coordinate rapid responses. Peptides, however, deliver precision instructions.
They bind to specific cellular receptors, activating intracellular signaling cascades that modify gene expression, enzyme activity, and energy utilization. This receptor specificity is what allows peptides for fat loss to influence appetite regulation without uniformly stimulating the entire endocrine system.
When metabolic imbalance develops , particularly insulin resistance, chronic inflammation, or stress-driven hormonal disruption and communication between organs becomes inefficient. The brain misinterprets energy availability. Fat tissue releases altered signaling molecules. The liver increases glucose production. Hunger signals intensify despite adequate energy stores.
Several therapeutic peptides that influence appetite regulation and metabolic signaling are being widely researched and discussed in metabolic medicine. These include:
• Semaglutide - a GLP-1 receptor agonist commonly studied for appetite regulation and glucose control.
• Tirzepatide (Mounjaro) - a dual GIP and GLP-1 receptor agonist that influences insulin signaling and satiety pathways.
• Retatrutide - a multi-pathway peptide that interacts with GLP-1, GIP, and glucagon signaling systems.
• BPC-157 - often discussed in regenerative medicine research related to tissue repair and inflammation modulation.
• TB-500 (Thymosin Beta-4) - studied in recovery and tissue regeneration contexts.
These molecules are being investigated for their ability to influence appetite signaling, metabolic efficiency, tissue repair, and energy regulation. Their physiological effects depend heavily on individual metabolic context, dosage, and clinical supervision. They should always be understood as regulatory signaling tools rather than standalone metabolic solutions.
Therapeutic peptides act as corrective signals within this disrupted communication network. Rather than forcing metabolic change, they help recalibrate signaling pathways that regulate satiety, nutrient partitioning, and fuel utilization.
Appetite Regulation: The Gut-Brain Axis and Peptide Signaling
Appetite is not a psychological phenomenon alone, it is rather a neuroendocrine process governed by the gut-brain axis. Signals from intestinal cells, adipose tissue, and circulating nutrients are integrated in hypothalamic centers that determine hunger intensity and satiety duration.
Certain weight loss peptides interact directly with this regulatory axis. They influence gastric emptying, satiety hormone release, and reward-driven food behavior. The result is not forced restriction but reduced physiological drive to eat.
Clinically, this effect is often described as reduction in food noise, the persistent cognitive and sensory pull toward food that many individuals with metabolic dysregulation experience continuously.
However, appetite suppression alone is not metabolic healing. Without restoration of insulin sensitivity, mitochondrial function, and inflammatory balance, appetite regulation remains temporary. This distinction is central to the iThrive Alive approach.
Among newer metabolic peptides, multi-pathway signaling molecules are receiving increasing scientific interest because they influence more than one regulatory axis simultaneously. Rather than acting only on hunger signals, some peptides also affect insulin response and energy expenditure demonstrating how interconnected metabolic regulation truly is.
Metabolic Efficiency: How Peptides Influence Energy Utilization
Beyond appetite, therapeutic peptides influence how the body processes and uses energy.
Metabolism is not simply calorie burning. It is the orchestration of glucose handling, fat oxidation, insulin signaling, and mitochondrial activity. In metabolic dysfunction, energy is stored inefficiently, oxidized poorly, and often diverted into fat accumulation.
Certain peptides for weight management solutions modify nutrient partitioning, the biological decision of whether incoming energy is stored or utilized. They may improve insulin sensitivity, enhance lipolysis, or increase cellular responsiveness to metabolic demand.
This is why some individuals experience improved body composition even when calorie intake changes modestly. The metabolic environment itself becomes more efficient.
Tissue Repair and Metabolic Restoration Are Connected
Metabolism does not operate independently from structural health. Muscle tissue, connective tissue, and organ integrity all influence energy regulation.
Peptides used in regenerative medicine such as those supporting ligament, tendon, and muscle healing indirectly influence metabolic function by improving movement capacity, reducing chronic inflammation, and restoring physical activity tolerance.
Repair-oriented peptides signal angiogenesis, collagen synthesis, and tissue remodeling. When injury recovery accelerates, physical activity becomes sustainable, which further improves metabolic health.
This illustrates an important principle: fat loss peptides do not act in isolation. Structural repair, inflammation control, and metabolic regulation are interdependent processes.
Clinical Insight: Mugdha Pradhan’s Metabolic Reset
Mugdha Pradhan, founder of iThrive experienced significant weight gain despite advanced nutritional knowledge. Emotional stress, nervous system overload, and persistent food-seeking behavior created metabolic conditions resistant to lifestyle change alone.
After extensive research into peptide physiology and metabolic signaling, targeted peptide therapy was introduced alongside structured nutrition, resistance training, micronutrient optimization, and nervous system regulation.
Over the years, Mugdha’s own health journey has evolved alongside her clinical work. Like many practitioners deeply invested in longevity and metabolic health, she has explored advanced regenerative tools including peptides in a structured, medically supervised manner.
Her transformation, however, was not about dramatic overnight change. It was about improving recovery, maintaining lean muscle, optimising metabolic markers, and supporting cellular repair. Peptides, when used appropriately and under guidance, can support signalling pathways related to regeneration, inflammation control, and tissue healing. But they are never a shortcut; they are adjuncts to disciplined nutrition, sleep, strength training, and stress regulation.
For Mugdha, the real shift wasn’t aesthetic; it was physiological. Better recovery, improved energy stability, sharper focus, and sustained muscle quality were markers that her internal systems were functioning more efficiently. The visible changes were a by-product of internal repair.
The outcome was not merely weight reduction but improved insulin sensitivity, decreased visceral fat, and restoration of appetite regulation. The intervention worked not because peptides replaced lifestyle but because they enabled adherence to metabolic healing protocols.
She is also clear that peptides are not for everyone and not a replacement for foundational health work. Gut health, micronutrient sufficiency, hormonal balance, and lifestyle remain the core pillars. Advanced tools only work when the basics are in place.
In Mugdha’s case, the therapeutic peptide used was Retatrutide, selected after extensive review of metabolic pathway research and clinical data.
Three biological factors made Retatrutide particularly relevant for her metabolic condition:
GLP-1 Pathway - Appetite and Satiety Regulation
Supported reduction in food noise, improved fullness signaling, and enhanced dietary adherence.
GIP Pathway - Insulin Efficiency and Nutrient Utilization
Helped improve glucose handling, metabolic flexibility, and hormonal coordination of energy storage.
Glucagon Pathway - Energy Expenditure and Fat Mobilisation
Supported increased metabolic activity and utilization of stored energy, contributing to body-composition change rather than intake reduction alone.
This multi-pathway signaling profile is what distinguished Retatrutide from earlier single-pathway metabolic peptides in her research process.
In her view, longevity is not about chasing biohacks, it’s about supporting the body’s natural regenerative intelligence with responsibility and context.
Her detailed experience is documented in the video:
“How I lost 16 kgs in 4 months - Mugdha Pradhan’s easy weight loss journey with GLP agonists.”
MOST IMPORTANT: It is important to note that the therapeutic effect observed was not attributed to the peptide alone. The intervention worked within a structured physiological framework that included nutrition planning, resistance training, micronutrient sufficiency, and nervous system regulation. The peptide functioned as a signaling facilitator that improved adherence and metabolic responsiveness.

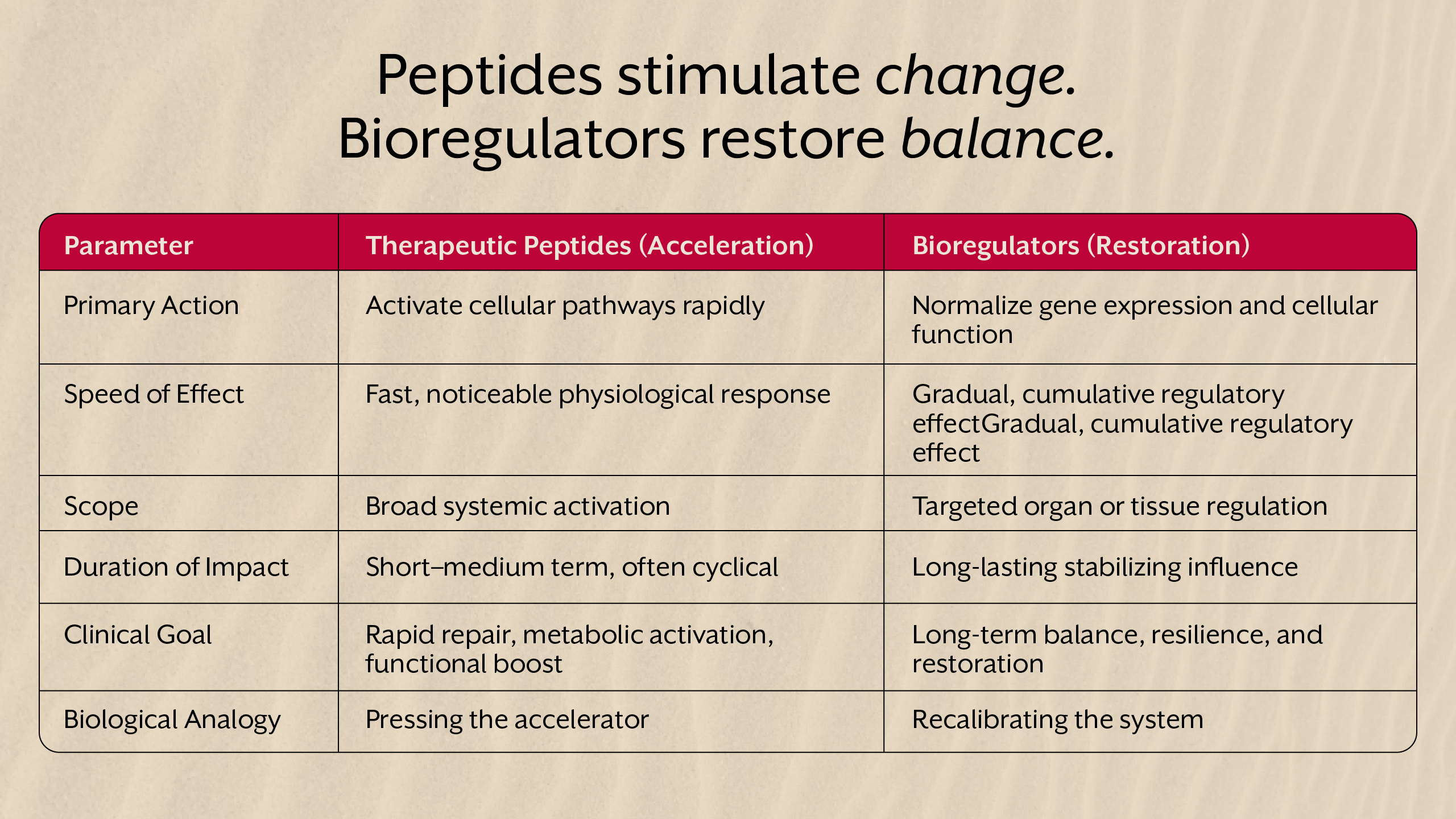
Peptides vs Bioregulators: Acceleration vs Restoration
Not all cellular signaling molecules operate similarly.
Therapeutic peptides typically accelerate biological processes. They stimulate pathways involved in repair, metabolism, or appetite control.
Bioregulators, in contrast, influence gene expression patterns more subtly. They restore cellular memory guiding tissues toward long-term functional balance rather than rapid activation.
In clinical decision-making, peptides are often used when rapid metabolic intervention is required, while bioregulators support sustained cellular normalization.
Understanding this distinction prevents misuse of powerful metabolic tools.
Why Peptides Alone Cannot Create Sustainable Fat Loss
Despite their powerful signaling effects, peptides for fat loss cannot compensate for poor nutritional status or metabolic dysfunction.
Protein deficiency, micronutrient insufficiency, circadian disruption, chronic stress, and inflammatory load all determine whether peptide signals translate into meaningful physiological change.
This is why iThrive Alive emphasizes foundational metabolic restoration such as nutrition planning, lifestyle restructuring, and targeted supplementation before advanced interventions.
Peptides amplify biological potential. They do not create it.
The iThrive Alive Philosophy: Precision Before Intervention
At iThrive Alive, peptide therapy is never approached as a universal weight management solution.
Clinical assessment evaluates fasting insulin, inflammatory markers, lipid patterns, stress physiology, sleep architecture, and nutrient status. Only when underlying metabolic drivers are identified does targeted intervention become meaningful.
This root-cause methodology ensures peptides are used as strategic metabolic tools, and not shortcuts.
Key Takeaway
Therapeutic peptides represent one of the most advanced developments in metabolic medicine because they function at the level of cellular communication. They influence appetite regulation, energy utilization, tissue repair, and neuroendocrine signaling with remarkable precision. Yet their true value lies not in rapid fat loss but in restoring biological responsiveness within systems already supported by nutrition, lifestyle, and metabolic correction. When used responsibly and within a root-cause framework, peptides can help recalibrate dysfunctional signaling networks that drive persistent weight gain. When used without metabolic foundation, they remain temporary metabolic accelerators rather than long-term solutions.
For clinical screening, metabolic assessment, or guidance on whether advanced peptide-based interventions are appropriate for your physiology, you may contact our team directly.
Email: care@ithrive.shop
📲 WhatsApp us directly for metabolic screening
All interventions are recommended only after structured metabolic evaluation and suitability screening.
Subscribe to our newsletter and receive a selection of cool articles every week



.png)


.webp)

.jpg)
.jpg)